Traumatic Brain Injury (TBI) is getting more attention than ever before. Media outlets have done a great job at highlighting the impact of TBI and Chronic Traumatic Encephalopathy (CTE) on football players. This extra attention and research are great news for anyone that’s experienced a TBI.
The reality is that TBI and CTE are not only found in football players. According to the Centers for Disease Control (CDC), in 2014, 2.87 million people ended up in an emergency room because of a TBI.
Neuropsychological evaluations for traumatic brain injury are one of the more common types of evaluations that we complete. Most of our patients are very anxious when they come and see us for an evaluation.
We want to help ease your anxiety and provide you with more information on what a TBI is and how it can impact you.
The goal of this blog post is to talk about the leading causes of TBI, how a TBI is diagnosed, how a TBI impacts your brain, and how a neuropsychological evaluation for a traumatic brain injury can help you.
What are the leading causes of Traumatic Brain Injury (TBI)?
The typical causes of TBI stay fairly consistent year over year.
Here are some stats from 2013:
- Falls, especially among young children and older adults, make up around 47% of head injuries.
- Blunt force trauma makes up around 15% of head injuries.
- Motor vehicle accidents make up around 14% of all head injuries.
- 65% are the result of car accidents.
- 15-20% are the result of motorcycle accidents.
- 10% are from bicycle accidents.
- Assaults (including child abuse) make up around 9% of head injuries.

You can read more about the leading causes of TBI here.
Every year in the United States over 50,000 people die as a result of a TBI. TBIs make up around 1/3 of all injury-related deaths.
Around 80,000 to 90,000 people a year experience a life-long disability as a result of a TBI.
We didn’t include all of these stats to scare you. We want to show you how common a TBI is and how many people it impacts every single year!
What are the types of Traumatic Brain Injury (TBI)?
TBIs are broken down into three types:
- Mild TBI (75-80% of cases)
- Moderate TBI (10-15% of cases)
- Severe TBI (10% of cases)
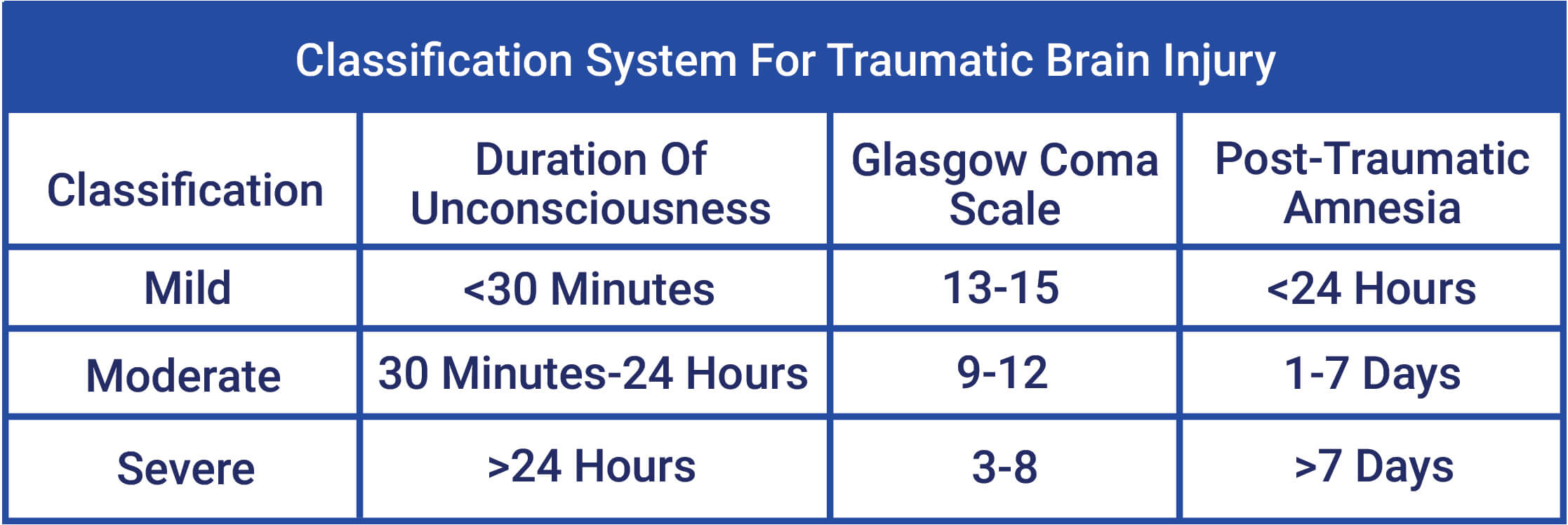
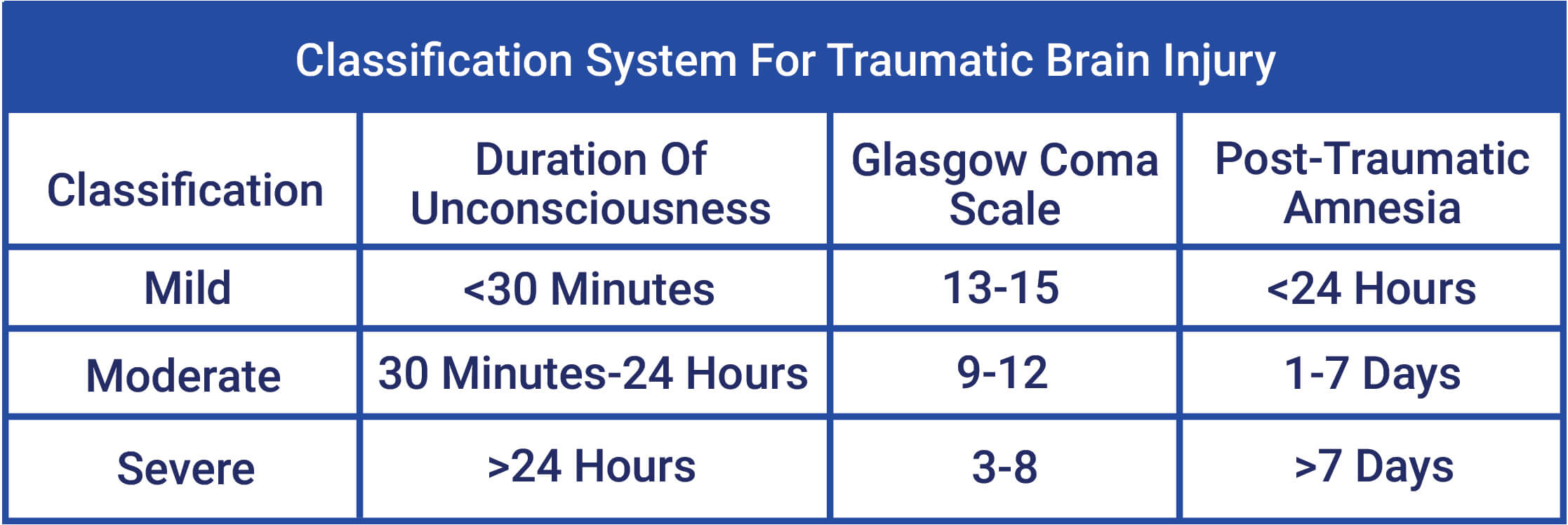
In order to determine the severity of the TBI, doctors use three criteria when they do their assessment in the emergency room.
- The Glasgow Coma Scale (GCS), which is determined when the person first arrives at the hospital.
- Loss of consciousness (LOC)
- Post-Traumatic Amnesia (PTA), which is a state of confusion and memory loss right after a TBI. PTA occurs because there is an impairment in attention and concentration, which are required to place new information into memory storage.
We’ve made a simple chart below to help break down how doctors determine the grade of the TBI.
What is Post-Traumatic Amnesia (PTA)?
Post-Traumatic Amnesia (PTA) is a state of confusion and memory loss right after a traumatic brain injury. PTA occurs because there are impairments in attention and concentration, which are required to place new information into memory storage.
Here are some of the common signs of PTA:
- Disorientation and confusion
- Anterograde amnesia (difficulty forming new memories)
- Retrograde amnesia (difficulty recalling old memories)
- Distractibility
- Difficulties with alertness
PTA causes individuals to have “islands of memory”. They can remember bits and pieces of the event but don’t have a continuous recollection of what happened.
They also have a hard time forming new memories (anterograde amnesia) and have difficulty remembering information BEFORE the event because of the disruption to their memory system (retrograde amnesia).
PTA ends AFTER the person has continuous awareness of their environment and is able to form new memories.
PTA is an important sign to be aware of because the length of the PTA can help us determine the severity of the TBI. The longer the PTA, the higher the likelihood that the TBI is causing memory impairment.
Here is what PTA looks like following a closed head injury.

What Are The Signs of a Mild Traumatic Brain Injury (mTBI)?
Mild traumatic brain injuries (mTBI) make up around 75-80% of all TBI cases.
An mTBI is the equivalent of a concussion. These two terms are often used interchangeably.
Typical signs of an mTBI include:
- Loss of consciousness less than 30 minutes
- GCS score of 13-15
- Post-Traumatic Amnesia (PTA) less than 24 hours
The most frequently endorsed symptoms in the initial days after injury are:
- Headaches
- Dizziness
- Fatigue
- Feeling slowed down
- Drowsiness
- Difficulty concentrating
- Subjective memory complaints
- Feeling mentally foggy
How Long Does It Take to Recover from an mTBI?
Individuals who experience an mTBI will perform poorly on neuropsychological tests up to a month afterward. That’s why we don’t recommend patients to see us until at least one month after their mTBI.
Luckily, people tend to recover very quickly from an mTBI. Most people recover anywhere from 1-3 weeks. In a very small percentage of cases, people can continue to present with signs up to 3 months after an mTBI.
If an individual experiences an mTBI but continue to report symptoms and memory complaints, then there are other factors that are causing the symptoms.
Depression, anxiety, or other unrelated factors such as life stress can impact attention, concentration, and memory.
It’s important to note that Mild TBIs generally don’t show up on CT scans or MRIs.
If an mTBI shows up on a CT or MRI, then it’s considered a complicated mTBI.
What’s a Complicated mTBI?
Complicated mTBIs cause more cognitive impairment than uncomplicated mTBIs. Their 6-month functional recovery pattern is more similar to the recovery period of individuals with a moderate TBI.
The good news is that 6 months post-injury, there are no notable differences between those with complicated and uncomplicated mTBIs on neuropsychological tests. The bad news is that those with a complicated mTBI have worse functional outcomes (e.g. more of an impact on their day-to-day functioning) compared to those with an uncomplicated mTBI.
Individuals with complicated mTBIs have worse outcomes 6-12 months post-injury compared to those with an uncomplicated TBI. Those with complicated mTBIs also have similar functional outcomes 3-5 years after the initial injury as individuals with moderate and severe TBIs.
What Are The Signs of a Moderate to Severe Traumatic Brain Injury (TBI)?
We’ve included both moderate to severe TBI under the same heading because they are along the same continuum.
Here is a breakdown of how we would differentiate a moderate TBI from a severe TBI.
Moderate and severe TBIs cause more impairments in cognitive functioning. The damage can be identified on CTs and MRIs.
The areas of cognitive functioning that are impacted depend on the region of the brain that is injured and the severity of the injury. We’ll go over some case examples later to demonstrate what a moderate or severe TBI looks like in real life.
Moderate to severe TBIs may include the following symptoms:
- Persistent headache
- Repeated vomiting or nausea
- Convulsions or seizures
- Inability to awaken from sleep
- Dilation of one or two pupils of the eyes
- Slurred speech
- Weakness or numbness in the extremities
- Loss of coordination
- Profound confusion
- Agitation and combativeness
- Memory impairment
- Sensory impairment
- Language impairment (problems with vocabulary, spelling, or comprehension)
- Behavioral and personality changes
- Poor attention, concentration, and information processing
How Long Does It Take to Recover from a Moderate or Severe Traumatic Brain Injury (TBI)?
This is a tough question to answer because there are a lot of factors that can impact recovery including the age of the individual and the severity and location of the injury.
There is research to support that individuals who have experienced a moderate to severe TBI can continue to recover from the injury for up to two years. Most of the recovery happens in the first year.
How much they improve depends on the severity of the injury and the regions of the brain that were damaged.
After three years, there is generally no substantial recovery of functioning. Unlike mTBIs, moderate to severe TBIs often result in permanent impairments in cognitive functioning.
What are the Causes of Traumatic Brain Injury (TBI)?
We’ve spent a bit of time talking about the different severity levels. Now we’re going to provide an overview of the two common causes of TBI.
There are two types of TBIs:
- Acceleration and deceleration injuries
- Crush injuries
What is an Acceleration and Deceleration Injury?
The most common cause of an acceleration and deceleration injury is the quick slowing that occurs in a car accident.
For example, in a car accident, the sudden slowing often causes individuals to hit their heads on their steering, dashboard, or side window.
In these cases, the individual’s head is propelled in one direction, then in the opposite direction, and then comes to a sudden stop.
If the acceleration/ deceleration is significant enough, it can result in a TBI.
Acceleration/ deceleration causes damage through three different mechanisms:
- Coup-Contrecoup Injury
- Rotational Forces
- Sudden Acceleration
We’ll talk about each of these injuries below:
Coup-Contrecoup Injury
In a coup-contrecoup injury, when force is applied to the skull (e.g. the person hits their head on a steering wheel), the brain is set into rapid motion.
This occurs because the brain is less dense (around the consistency of toothpaste or Jell-O) than the skull.
The brain is surrounded by cerebrospinal fluid (CSF) and is essentially floating in the skull like a buoy in the ocean. CSF helps protect the brain from injury by acting as an airbag, but if the forces are too much, the CSF can’t protect the brain from hitting the skull.
The “coup” is the injury that occurs when the brain hits the bony inside portion of the skull (called the calvarium). This is the first point of impact. The “contrecoup” is when the brain goes in the opposite direction and hits a point on the opposite side of the skull.
For example, in a car accident, an individual might hit their forehead on the dashboard or steering wheel. The brain will suddenly move forward in the skull and hit the front portion of the skull (coup) and then suddenly move in the opposite direction and hit the back portion of the skull (contrecoup).
The presence of a coup-contrecoup injury indicates that the force of the impact was strong enough that it caused two points of bruising.

This type of injury often results in contusions or bruising of the brain. This occurs because the inner contours of the skull have bony protuberances and are not smooth.
The brain is essentially flung against these bony protuberances which cause bruising and tears in the brain tissue.
The regions of the brain that are most commonly impacted are the inferior frontal lobe and the anterior (front) portion of the temporal lobes. This occurs because the interior portions of the skull in these areas have irregular surfaces and bony protuberances.
Rotational Forces
Rotational forces are created when the head is struck at an angle causing the brain to twist away from the point of impact.

The rotational forces cause the fibers and blood vessels in the brain to rotate and twist resulting in damage.
The brain fibers that stretched are the white matter axons. This occurs because the white matter is less dense than the gray matter and is more susceptible to injury when rotational forces are applied. When stretched to the point of breaking, they are sheared and cause diffuse axonal injury.
Sudden Acceleration
When the brain is set into sudden and violent motion, it can be damaged by the sharp and bony protuberances that are inside of the skull (called the calvarium).
These protuberances are located in the region of the skull that houses the inferior frontal lobe and anterior temporal lobes.
These regions are the most susceptible to damage when the brain subjected to sudden acceleration.
What kind of damage can an Acceleration and Deceleration Injury Cause?
The specific type of injury tends to produce a predictable pattern of damage and a certain type of neuropsychological profile.
In general, coup-contrecoup types of injuries tend to impact the frontal lobe and the anterior portions of the temporal lobes. The severity of the damage depends on how strong the force of the impact was.
Rotational acceleration causes diffuse axonal injury and damages the white matter regions of the brain. The severity damage depends on the strength of the rotational forces.
Since most TBIs cause damage to the white matter, interior frontal lobe, and anterior temporal lobes, the pattern of impairment in behavior, cognition, and emotion are predictable to a certain extent.
Knowledge of these patterns can help us determine if the disturbances in cognition or behavior are due to the TBI or external factors such as another condition or an exaggeration of symptoms.
Inferior Frontal and Anterior Temporal Lobes
The inferior frontal lobe and anterior temporal lobes are involved with executive functions such as the control and regulation of cognition, behavior, and emotions. Impairments in cognition can cause individuals to have difficulty with attention, focus, and multitasking. They can also be easily distracted and will often lose their train of thought.
Contusions to the surface of the anterior temporal lobes can cause sudden and unexpected bursts of anger, memory impairment for recent events, depression, hallucinations, rapid mood swings, and epileptic seizures.
Damage to the orbitofrontal region of the frontal lobe results in impairments in behavioral and emotional regulation can cause individuals to engage in impulsive or excessive behaviors, inappropriate or aggressive behaviors, and have sudden and unexpected mood swings.
In more severe cases of TBI, there can be damage to the dorsolateral and ventromedial regions of the frontal lobe.
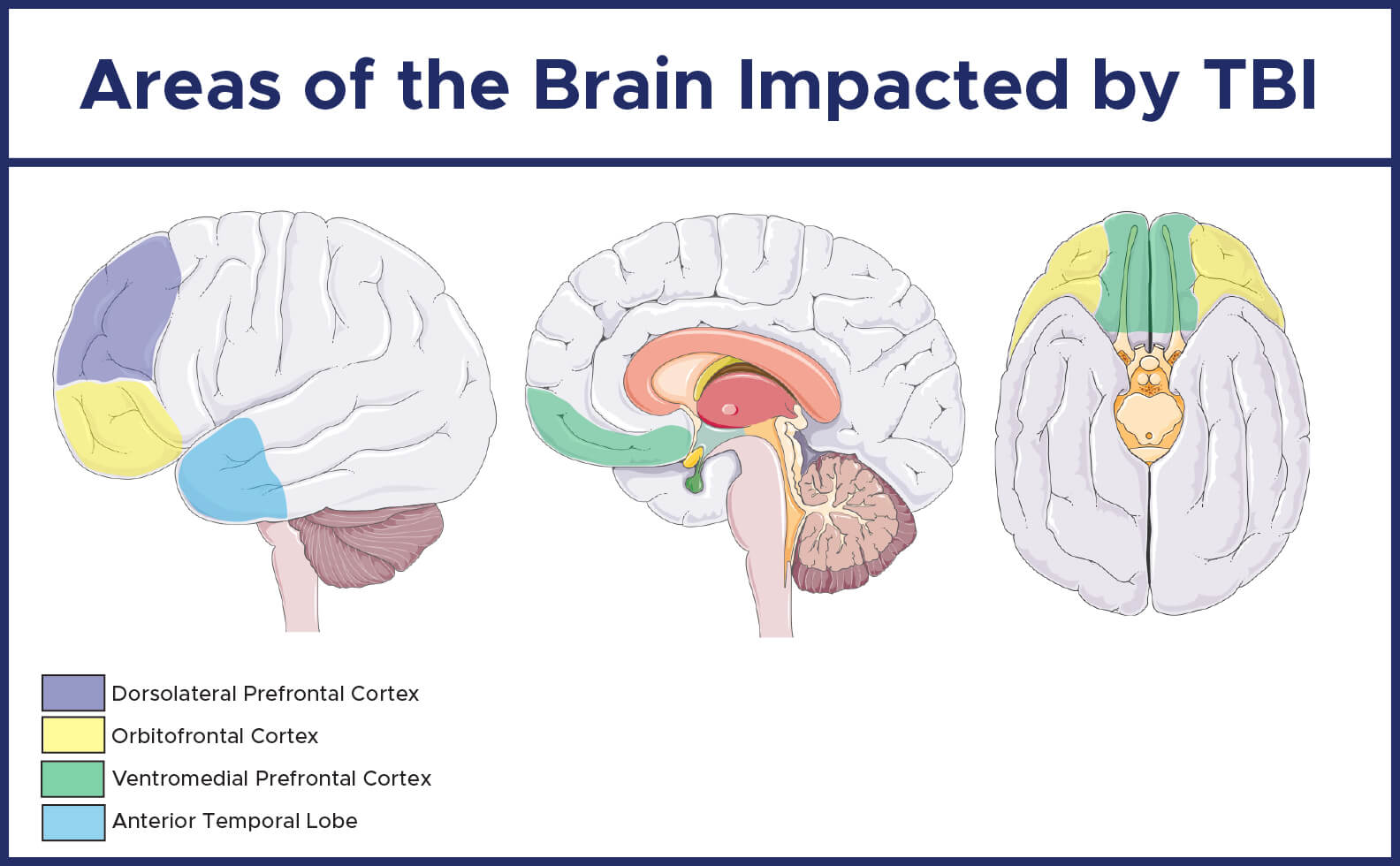
Damage to the dorsolateral region of the frontal lobe results in impaired judgment, reasoning, problem-solving, planning, and cognitive flexibility. Individuals can also be easily distractible, have poor attention and concentration, have difficulty learning from experience, and have difficulty accurately recalling information from memory.
Damage to the ventromedial region of the frontal lobe results in diminished drive, decreased motivation, loss of pleasure from the environment and individuals can also appear apathetic (feeling indifferent or lacking emotion). These individuals are often incorrectly diagnosed with depression since many of these symptoms are also seen in individuals with major depressive disorder.
In the most severe cases, all three regions (dorsolateral, orbitofrontal, and ventromedial) can be damaged and can cause impairments in the following areas:
- Impaired executive functioning (e.g. planning, reasoning and flexibility of thought and behavior)
- Disinhibition (e.g., impulsivity, lack of restraint, distractibility)
- Apathy (e.g., passivity, lack of drive, diminished motivation)
Diffuse Axonal Injury
The brain has a white tint to it because of the fatty myelin sheath that covers the axons in the brain. Axons are fibers that transmit impulses from one neuron to another.
The fatty myelin sheath helps insulate the axons and increase the transmission speed of the axons. Axons are similar to the electrical wires in a city that help transmit electricity from a power station to your house.
In diffuse axonal injury, the rotational forces shear the white matter (the myelinated axons). When there is damage to the white matter (the myelinated axons), the various regions of the brain are not able to communicate as efficiently with one another.

This means that an individual with diffuse axonal injury will have problems maintaining their train of thought, gathering thoughts, and processing their thoughts.
Their thought process will also become slow and inefficient and they will have to concentrate much harder than they normally would to complete tasks. Since they have to concentrate harder, they tend to get mentally fatigued quicker.
What is a Crush Injury?
Crush injuries are another form of blunt force trauma. In a crush injury, the head isn’t propelled into motion. It stays stationary and is struck with a moving object.
Examples of crush injuries include being hit by a falling object (e.g. a tree branch or object at a construction site) or being kicked in the head during an assault.
If the head is struck hard enough or is struck from the side, it can cause the brain to propel forward inside of the skull and cause the acceleration/ deceleration type of injury we discussed earlier.
If the head is not struck hard enough to cause the brain to propel forward, then the damage is generally going to be in the area directly below the point of impact. In this case, the brain isn’t propelled forward so there won’t be diffuse axonal injury (there can be axonal injury at the site of impact) and there won’t be a coup-contrecoup injury.
The acute (immediate) and chronic (long-term) neuropsychological profiles of a crush injury are different than the profile of an acceleration/ deceleration injury.
Immediately after the injury, there might not be any significant alteration of consciousness and there is rarely any prolonged confusion or disorientation. There might be a brief loss of consciousness depending on the force of the impact.
For example, if the vertical force is strong enough to push the brain downward to either crush or damage the brain stem (which is responsible for arousal and alertness), then there will be a loss of consciousness.
The chronic neuropsychological profile of a crush injury tends to be more localized and causes impairments in the areas of the brain directly below the site of impact. You generally won’t see impairments in executive functioning due to damage to the frontal and temporal lobes or slowness or loss of train of thought due to diffuse axonal injury. The only exception to this would be if the crush injury happens to be in the frontal or temporal lobes.
Conclusion
Neuropsychological evaluations for traumatic brain injury (TBI) are one of the more common types of evaluations that we complete. The degree of impairment can vary depending on the severity of the TBI (mild, moderate, or severe).
Acceleration/ Deceleration injuries tend to impact executive functioning due to damage to the frontal and temporal lobes and cause slowness or loss of train of thought due to diffuse axonal injury.
Crush injuries typically cause localized impairment in the areas of the brain directly below the site of impact.
Neuropsychological testing can help determine the areas of the brain that are impacted by a TBI and how these impairments are impacting your day-to-day functioning. More importantly, testing can also determine how other factors (e.g. depression, anxiety, life stress) are impacting your cognitive functioning.
We specialize in conducting comprehensive neuropsychological evaluations for traumatic brain injury.
Our evaluation can determine how a traumatic brain injury is impacting your day-to-day functioning and provide treatment recommendations to help improve your quality of life.


